We have therefore decided
This is the really breathtaking bit – the brand new CEO of the hospital telling the patient “we don’t share your beliefs so we’ve decided not to do your surgery.”
I think she might very well get fired for that, and perhaps more than fired.
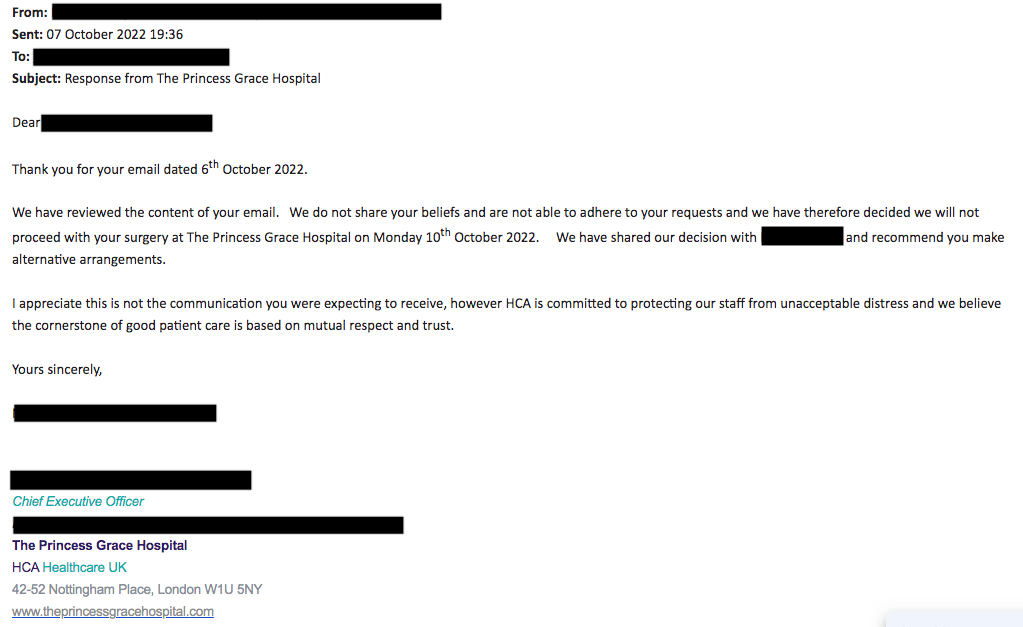
It’s a quite incredible thing to say – to put in writing. I think it screams lawsuit.

So, is this the Royal We, or would a FOI request come up with notes from a meeting convened to discuss the issue? More heads for rolling?
If you respected patients, you would not lie to them. You would not allow men pretending to be women on your staff. How can patients trust a facility where this kind of imposture is tolerated? Why should a staff member’s desire for “validation” override a patient’s need for care? Why does this one tiny group get to dictate and enforce a policy that ends up allowing them to bring their fetish into the workplace? How is that respectful or trustworthy? It’s the medical equivalent of letting TiM police officers frisk female prisoners.
As a retired surgeon I have a couple of observations. It’s true we don’t differentiate care based on our preferences, at least in trauma care where I practiced.
First, something seems off with how this is clinically described. It’s referred to as a life-saving emergent condition, but the patient was sent home (presumably to administer a routine bowel prep in anticipation of surgery based upon the timing). That’s not how emergent situations are handled. Patients aren’t sent home to prep for emergency surgery. So, at first glance this sounds like an elective or planned surgery (which can of course be for dangerous diagnoses). Without a diagnosis it’s hard to put this in the right perspective. I’m not condoning the behavior exhibited but without all the facts I can’t say for sure that cancelling the procedure is an ethics violation.
There are rare situations where patients are ‘fired’ though not of course in the midst of a true emergency. It would be interesting to know the specifics of the diagnosis, though I may have missed it.
Second, It appears that this was decided by the hospital NOT the attending surgeon. Sounds from the letter that they were informed of this decision as well. Unless they have surgical privileges at another hospital there would be nothing immediately they could do.
Finally, I happened to train at a hospital which employed a transgender person who was the second person in the world to have gender altering surgery (in Europe) in the 1980’s. This was in the Midwest in the 1980’s so you can imagine it wasn’t particularly mainstream.
Pliny, where is it described as emergent? Acute, life-saving, but not emergent, at least not initially. I may have missed it but I didn’t see it.
Patient has “already had one emergency admission with a perforated intestine recently.”. And the “…. procedure is particularly complex and requires a robot and two surgeons.”
“With the operation cancelled, probably the only alternative available to her at this, now, late stage, is open surgery, something her surgeon did not recommend as the best option.”
Patient was in A&E four days *after* her surgery was originally to take place, and “may now be too weak to have the open surgery.”
Finally, it’s the CEO who is being accused, not the surgeons.
‘Acute lifesaving’ generally means emergent, at least in the US.
I find it unlikely that in all of London there’s only one facility able to perform advanced laparoscopic surgery if that is what is required. Portland is a considerably smaller city and there are at least 4 top-flight centers able to provide that type of care.
After reviewing cases for 30 years I’m pretty sure there’s something crucial missing from this discussion. It’s not unusual particularly when the clinicians aren’t going to breach confidentiality to fill in gaps. It doesn’t all add up.
Earlier commenters alluded to concerns about MD ethics in this situation.
I know, Pliny, it seems implausible. But it also seemed implausible to me that my sister had her son in a large hospital in Little Rock where they had ZERO surgeons who could do an emergency C-section, so I’m always prepared to accept that there might be some weirdness happening. In my sister’s case, when the cord wrapped around the baby’s neck, and there was no one to deliver the baby (in a hospital that has an OB ward?), the baby was born with cerebral palsy. The hospital then changed its records to indicate that the cord wrapped around the baby’s neck only minutes before delivery, but my sister and her husband had documentation that it had been much longer. No lawyers would take the case, because they said a jury would be more inclined to believe evidence presented by the hospital.
So…I always wobble along the tightrope in these cases, because it seems so implausible that they couldn’t transfer her to another hospital (which they said they couldn’t), or bring in a surgeon who could do a C-section.